This post is part of the accompanying tips, resources, interviews with experts, and stories of recovery included in the exclusive serialization of Cured: The Memoir.
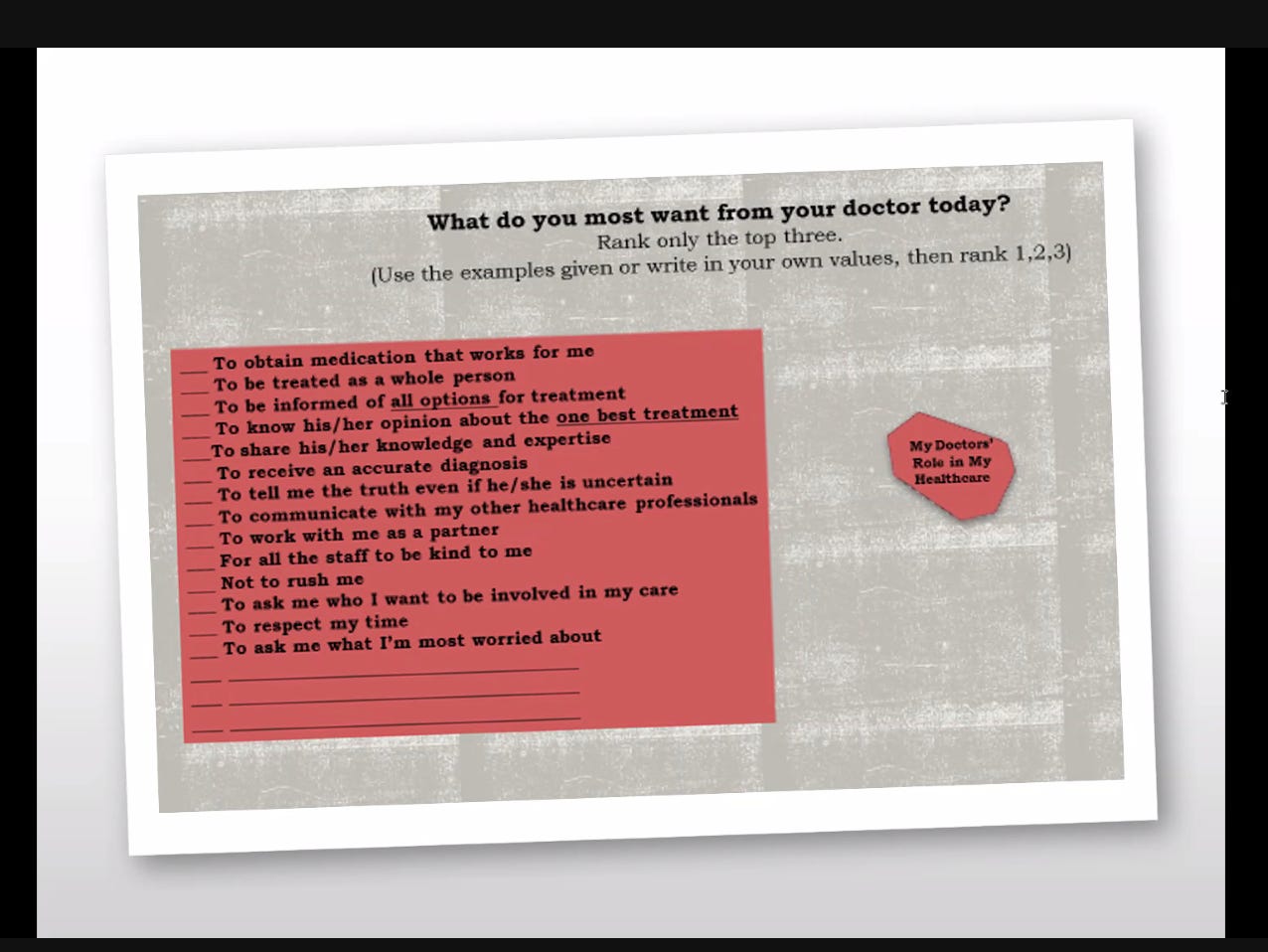
Today, I bring you the shared decision-making card developed by Yale’s Maria O’Connell and Janis Tondora (and others like it) changes the way we enter into and receive treatment from passive to active.
How many of us feel comfortable telling a physician what you need and want in your care? What about a psychiatrist or other mental health professional?
Our current mental health system is designed around the idea that the clinician is in charge and the patient is the passive recipient of care. (This is no one’s fault; it’s simply the system we have at present.)
Enter the Shared Decision-Making Card developed by Maria O’Connell and Janis Tondora, both professors of psychiatry and researchers in the Program for Recovery and Community Help at Yale School of Medicine. (To learn more about their incredible work, click on their names.) A clinician can’t be everything and all to us, and he/she/they can’t know what we need if we don’t tell them. With the Shared Decision-Making Card, we mark the three most important things to us:
You can amend these as needed and use them in appointments with any physician or mental health professional (therapist, psychologist, social worker, etc.).
This card gives us a chance to consider what we want from our treatment before we enter the office or examination room. It also gives us agency so we’re in a partnership with our doctors and mental health professionals.
For two decades, studies have shown that treatment tailored to patient preferences is associated with
greater engagement in treatment,
improved therapeutic alliance,
increased patient satisfaction, and
improved outcomes of care.
I asked O’Connell if it was a bit like the allergy card my niece hands the server when we eat at a restaurant. My niece doesn’t have to explain. It’s all on the card. O’Connell responded, “It’s exactly like that.”
O’Connell and Tondora stress how important this could be for someone in crisis. And think how effective this could be for young people—or any of us—in preparation for when we have to articulate our needs and can’t do so.
To get the best treatment, we can’t expect our clinicians and mental health professionals to do all the work. We have to create our own care.
Readers like you make my work possible. Support independent journalism by becoming a paid subscriber for $30/year, the equivalent price of a hardcover book.
Visit the Table of Contents and Introduction of Cured:
Find more resources for mental health recovery.
Read the prequel to ‘Cured,’ ‘Pathological’ (HarperCollins):